

Peters et al 12 examined 50 subjects with a do-not-intubate directive and with hypoxemic respiratory failure who received HFNC and many subjects did not need to escalate to NIV. In end-of-life situations, there are few studies that attempt to compare HFNC with other treatment strategies and the majority of them compared with NIV.
#High flow oxygen at home Pc
These physiological and clinical effects, specifically the comfort of the technique which is also reported to be more comfortable than COT and NIV, 11 indicate its potential outside the intensive care unit, namely in the PC context. 10 In fact, in exacerbated COPD patients studies have already shown that HFNC is able to keep PaCO2 unmodified, while oxygenation slightly deteriorates as opposed to NIV and also the work of breathing is reduced with HFNC by a similar extent to NIV, while it increases by 40-50% during COT. 7, 11Ĭlinically, HFNC effectively reduces dyspnea and improves oxygenation in respiratory failure from a variety of aetiologies, thus avoiding escalation to more invasive supports.

Physiologically, HFNC maintains the integrity of mucociliary function by delivering heated and humidified gas at natural body conditions, it reduces the anatomical dead space, improves carbon dioxide wash-out, reduces the work of breathing, generates a positive end-expiratory pressure and a constant fraction of inspired oxygen.
#High flow oxygen at home skin
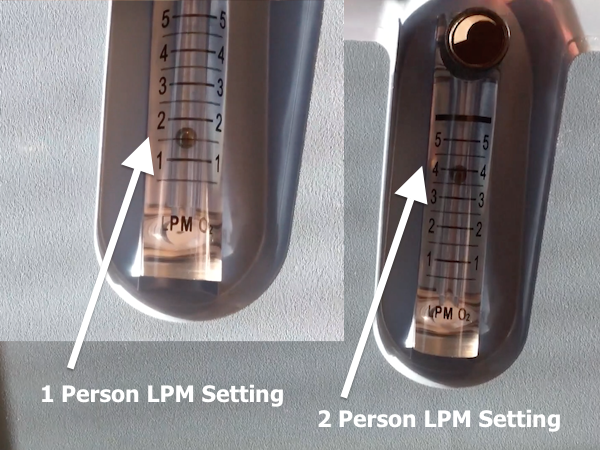
HFCN therapy has specific indications and has some advantages in relation to COT or NIV because it can be less claustrophobic, produces less skin breakdown, and does not impede respiratory patients from eating or talking. Related to COT and NIV a new oxygen therapy has emerged, high-flow nasal cannula oxygen (HFNC) designed to provide oxygen at high flows with an optimal degree of heat and humidification, which is well tolerated and easy to use specially in the intensive care unit but in PC setting it is still very limited. The rationale for end-of-life NIV should be to provide comfort and relief of dyspnea, but the use of NIV in patients with an order for non-resuscitation remains controversial, largely due to the lack of clarity in the defined end-of-life objectives. As there is no clear evidence of symptomatic benefit of palliative oxygen in the literature its use should be on an individualized basis and the role of NIV as palliative treatment is still very uncertain. 9Īt the end-of-life the delivery of oxygen can be made by conventional oxygen therapy (COT) or by non-invasive ventilation (NIV). Its known that there are a range of treatment strategies for dyspnea both pharmacological and non-pharmacological to ensure symptomatic relief, 7 oxygen therapy being one of them but according to PC research and recommendations the routine use of oxygen treatment for shortness of breath is not recommended 8 and it is imperative to determine whether the use of the so-called “Palliative oxygen” is appropriate. The proactive involvement of PC in respiratory patients like those with severe COPD has already been shown to have a positive impact and among them dyspnea is the most prevalent symptom, which can be quite disabling at all levels and enhanced by several factors reflected in PC in the concept of “total dyspnea”. Its recognised that PC in the last 4 decades has pioneered symptomatic control and has addressed end-of-life issues / decisions in patients with neoplastic pathology, but little attention has been given to patients with progressive and irreversible chronic respiratory pathologies with limited / reserved prognosis. 2 This highlights the importance of providing palliative care (PC) with a holistic approach, focusing on the quality of life of patients and their families, preventing and relieving suffering in respiratory patients as presented by Martins et al. In the course of time chronic respiratory diseases lead to severe symptomatic burden for patients which reflects on their family members and society and with high health costs associated. 2 Indeed, according to the World Health Organization COPD is already considered the third leading cause of death worldwide. Chronic respiratory diseases are prevalent among hundreds of millions of people in the world 1 and their prevalence in Portugal is increasing, with asthma and Chronic Obstructive Pulmonary Disease (COPD) being the most prevalent.


 0 kommentar(er)
0 kommentar(er)
